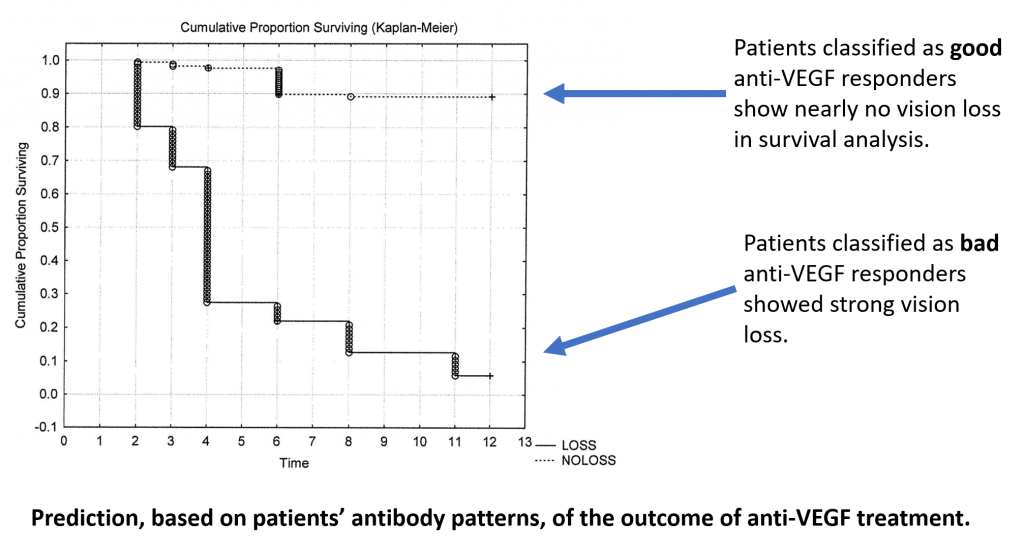
In several clinical studies, we were able to detect autoantibodies that are differentially regulated in AMD patients responding to anti-VEGF treatment, compared to non-responding patients who continue to lose their vision. These altered autoantibody profiles allow us to predict whether a patient will respond to treatment with anti-VEGF or not.
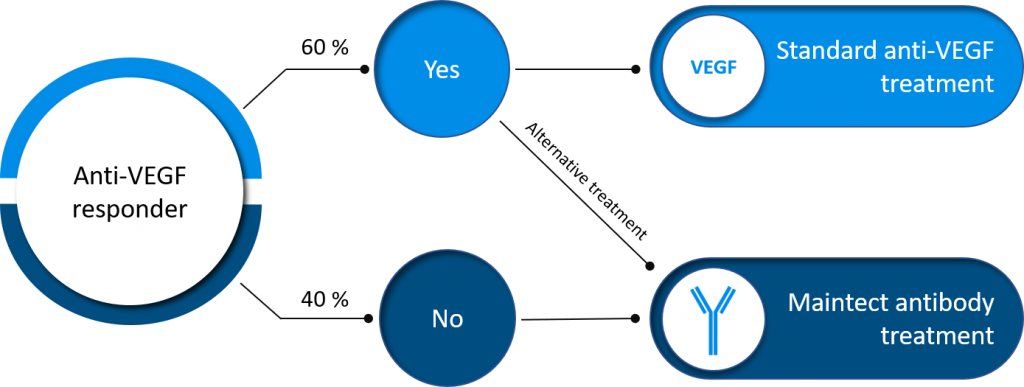
Based on these results we are developing a saliva-based diagnostic lateral flow assay (LFA) for AMD based on these altered autoantibody profiles, as a „Companion Diagnostic“ to guide subsequent treatment decisions. The test results can categorize patients into responders, reduced responders and non-responders to anti-VEGF treatment. For reduced responders, more anti-VEGF injections or synergistic application of another antibody is a possibility. For non-responders, the expensive anti-VEGF treatment can be stopped, and an alternative strategy applied.
Alternative Treatment
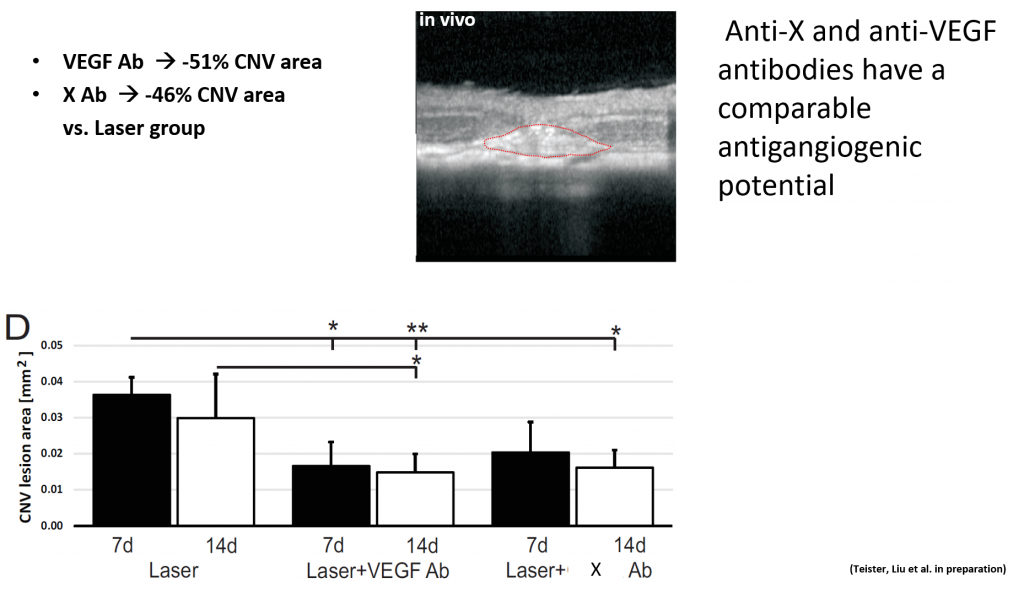
While working on the companion diagnostic LFA and in light of the variable response to the current gold standard anto-VEGF treatment strategy, we have developed our own antibody therapy for non-responders. Differences in the autoantibody profiles of wet AMD patients vs control patients, an alternative target for treatment was found. In in vivo and in vitro studies, the maintect antibody showed very promising results for treating AMD in two different animal models.
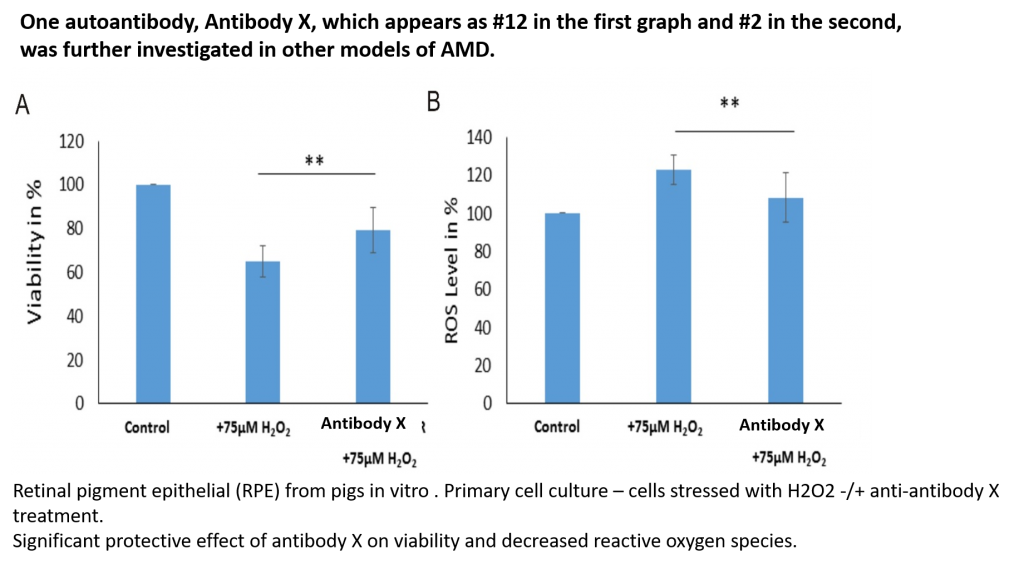
Firstly in vitro studies in H2O2-stressed retinal pig epithelial cells revealed that the antibody had a significant protective effect on cell viability as well as decreasing reactive oxygen species. This is important as AMD affects these cells. Secondly, in vivo studies in a mouse AMD model showed an antiangiogenic effect of antibody 125 in compareable to the gold standard anti-VEGF treatment. These very promising results point to an alternative treatment of AMD, by targeting a completely new therapeutic pathway.
Antibodies present, or not, in dry or wet AMD are therefore promising targets to be tested as new therapeutic options for non-responders to current treatment options. This applies not only to the whole antibody, but also to its paratope sequences (CDR-sequences) which may also be developed as therapeutic molecules, but without the problems often associated with whole antibody treatment. Paratope sequences could be sequenced and synthesized more easily and would offer a more cost-effective alternative to antibody treatment. In addition, our results with the autoantibody profiles of AMD patients, also provides valuable information about the metabolic pathways involved in the disease. This opens the door to specific drug therapy that targets these pathways, as an alternative to antibody therapy. Thus, the immunological changes found in AMD patients offer a way to personalize therapy in order to offer each patient the most promising treatment.
The Future
AMD is usually diagnosed in the late stages when visual loss is already present. At maintect GmbH, we continue to look for markers that allow early diagnosis of AMD, both the dry and wet form. Furthermore, we want to be able to distinguish the two different forms of AMD with a quick and easy to use point-of-care device.
In addition to establishing an early diagnostic tool for dry AMD, the determination of the risk of conversion from dry AMD into the wet form is another key goal on our path to a personalized and optimized AMD therapy.
- Joachim SC, Bruns K, Lackner KJ, Pfeiffer N, Grus FH. Analysis of IgG antibody patterns against retinal antigens and antibodies to alpha-crystallin, GFAP, and alpha-enolase in sera of patients with „wet“ age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 245:619-26, 2007
- Franz Grus, Christina Korb, Norbert Pfeiffer. Predictive Markers Useful in the Treatment of Wet Age- Related Macular Degeneration. Patent US2019072550 (A1).
